The New Jersey Hospital Association (NJHA) Center for Health Analytics, Research, and Transportation (CHART) reports that social determinants of health play a part in who gets sick and who dies from the virus.
By Katrina Janco | May 31, 2020
While novel coronavirus (COVID-19) has had its heaviest impact on seniors and those with underlying health conditions, early reports from New Jersey health researchers seem to indicate that the virus has also disproportionately affected communities of color.
Researchers at the New Jersey Hospital Association (NJHA) Center for Health Analytics, Research, and Transformation (CHART) studied the demographics of 12,581 patients discharged from hospitals after having been treated for COVID-19 since April 1.
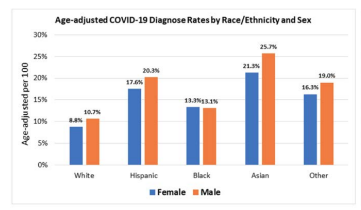
After adjusting for the ages of those patient groups, they discovered that those of Asian ancestry had the highest rates of COVID-19 diagnoses, followed by Hispanic people.
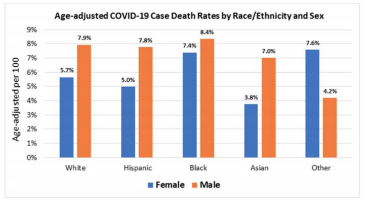
Black New Jerseyans were among those most likely to have died from COVID-19 complications, with black men at significantly higher mortality rates than black women, even though more black women were diagnosed with COVID-19 than their male counterparts.
These preliminary findings are consistent with broader national trends illustrating racial disparities in COVID-19 infection and mortality rates across America, and can be explained by exploring the social determinants of health in the communities affected.
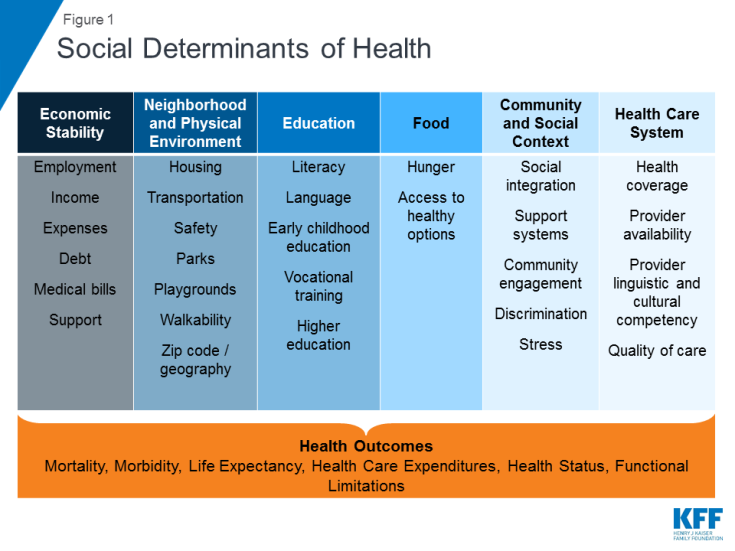
Defined by the World Health Organization as “the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life,” social determinants of health have been studied by public health experts for decades.
The same communities of color that historically have suffered health concerns at higher rates than white communities are also facing higher risks for contracting COVID-19 and potentially dying from it.
Just a few of those social determinants include: facing more barriers to accessing health care and health insurance, working low-paying-yet-pandemic-essential jobs, or living in housing that doesn’t allow for social distancing. To overcome those disparities, NJHA has pledged to tailor its approach to communities of color in acknowledgment of the challenges they face.
“It really does take a village to keep our communities healthy,” said Sandy Cayo, NJHA vice president of clinical performance and transformation.
“In each community, we need to work with trusted partners to see the vulnerabilities of certain groups and plan the actions we’ll need to keep them safe,” Cayo said.
When NJHA community partners like YMCA raised the issue that people living in transitional housing were at greater risk of contracting the virus, NJHA worked with hotel chains to provide temporary shelters that would allow them to social-distance.
A lack of COVID-19 information for non-native-English speakers has been another risk factor for communities of color.
As one of the most culturally diverse states in America, New Jersey must provide accurate, widely available public health messages in a variety of languages, especially in a time of emergency, Cayo said.
Work is also being done to ensure accessible resources for the deaf and hard of hearing, as evidenced by the inclusion of American Sign Language translators during state press briefings.
Finally, those disproportionately affected by COVID-19 may need additional help to quarantine safely, and to access mental health and child and family supports, for all of which CHART advocates.
“Even now, as the virus is still revealing itself, we are seeing new areas of concern related to how COVID-19 impacts people based on age, gender, the presence of different chronic conditions, or even factors such as vaping or tobacco use,” Cayo said.
“Most definitely, we are interested in the impact of social determinants like housing, transportation and socioeconomics on COVID-19 outcomes,” she said.
CHART is also working to address implicit bias in medical settings, which has been strongly shown to result in poor health outcomes in communities of color, particularly among black Americans.
“This initial data analysis wasn’t designed to provide that type of information yet, but there will be additional research in the months to come to glean insight and develop actions that can improve our response and our outcomes in future viral outbreaks,” Cayo said.
Last spring, NJHA began its “Patients, Prejudice and Policy” conference series “to help raise awareness and self-reflection about biases in ourselves and in our institutions,” and continues to be area where the association is “pursuing additional learning opportunities,” Cayo said.
“We know we can’t improve the health of the people of New Jersey without recognition and action on the underlying social determinants of health,” she said.