In a press briefing Wednesday, New Jersey Deputy Commissioner for Public Health Dr. David Adinaro spoke with reporters about how the state is handling the latest COVID-19 variant.
By Matt Skoufalos | January 6, 2022
Even after nearly two full years of the novel coronavirus (COVID-19) rampaging across the state, New Jersey faces record numbers of new infections at the outset of 2022.
“We’re in a new and different phase of this pandemic,” said Dr. David Adinaro, Deputy New Jersey Commissioner for Public Health, in a media briefing Wednesday.
New Jersey is taking on tens of thousands of new cases daily, with positivity rates approaching 60 percent at the end of December 2021.
That infection spike is attributable pretty exclusively to the SARS-CoV-2 (COVID-19) variant B.1.1.529, “Omicron,” which was designated a “variant of concern” by the World Health Organization (WHO) November 26, 2021.
Viral variants are identified through genetic sequencing tests that, when performed rapidly and at scale, can help researchers around the world track the evolution of a disease like COVID-19, and use that information to develop more effective interventions against it.
In April 2021, the United States first began tracking cases of the B.1.617.2 “Delta” variant, which was more infectious and virulent than variants that emerged in the earlier waves of the pandemic. After just a few months, Delta-variant COVID-19 accounted for nearly every case of the virus in the country.
By late November 2021, however, public health officials confirmed the first Omicron variant COVID-19 cases in New Jersey. Since that time, Omicron has “out-competed” Delta, Adinaro said, and now is believed to account for as much as 95 percent of cases in Region Two of the federal Agency for Toxic Substances and Disease Registry (ASTDR), which includes New Jersey.
“Thirty-five percent of everything that we sequenced in the first two weeks of December were Omicron [cases],” Adinaro said.
“Pretty much, if you’ve been infected with COVID now, you have Omicron; if you were infected in October, you had Delta,” he said.
Omicron more infectious, less severe than Delta, but caseloads loom
Symptomatically, Omicron-variant COVID-19 can present with fever, body ache, and fatigue; as compared with Delta-variant COVID, patients with Omicron-variant COVID are complaining more of headaches and sore throats instead of respiratory issues.
Some still lose taste and smell, as well; however, and more importantly, Omicron-variant COVID is better than Delta-variant COVID at “evading antibodies” generated by a prior COVID-19 infection or even a vaccination, Adinaro said.
“Despite that, the seriousness of the disease it causes is less than what we’ve seen in Delta,” he said.
“If you took the same number of people who were infected with Delta and Omicron, you would see more hospitalizations in the Delta group, [and] you would see more significant symptomatic disease in the Delta group.”
Although people infected with Omicron-variant COVID “feel pretty miserable,” Adinaro said, they’re less likely to be hospitalized with the kinds of respiratory concerns that Delta-variant COVID produced.
“The problem,” Adinaro said, “is the sheer number of people who are now becoming infected.”
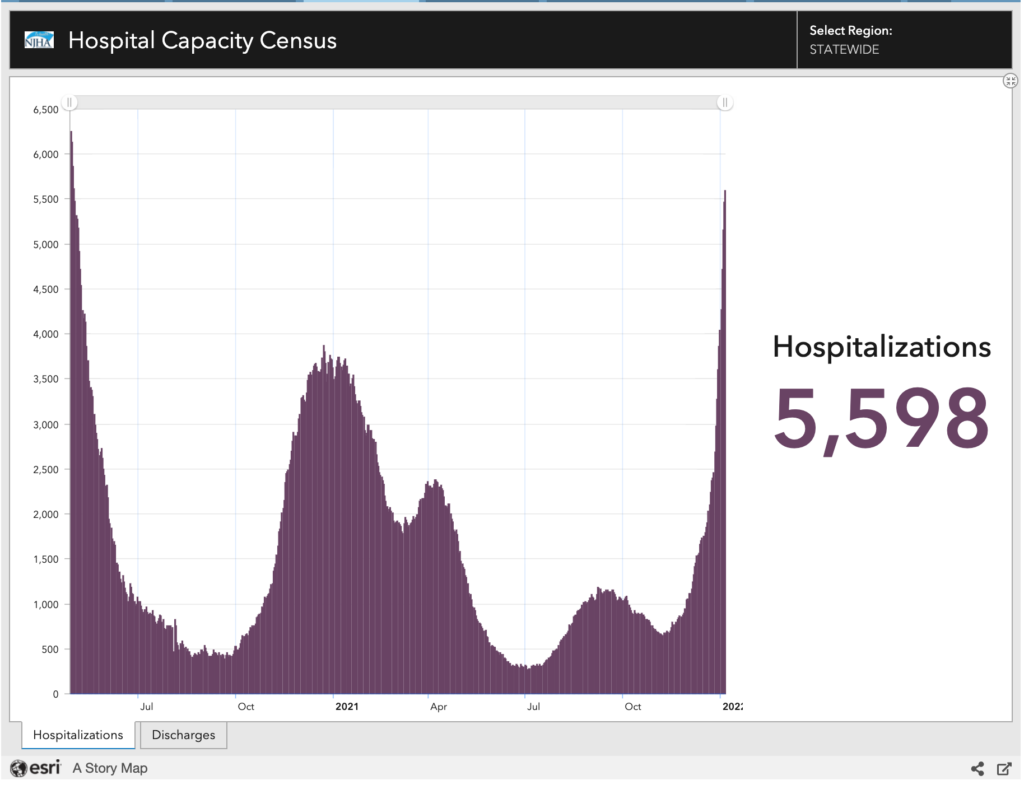
As of January 5, nearly 5,600 New Jerseyans are hospitalized, a figure approaching levels last seen in late April 2020, during the earliest stages of the pandemic. That’s especially troubling, Adinaro said, because the 72 hospitals across the state are also busy caring for people with chronic diseases and seasonal flu.
“As opposed to last year, where we had very little, if any flu, we’re already in the moderate category for influenza, and that kind of lines up with what we saw in 2019 and 2020,” Adinaro said.
“We were fortunate, I think, that distancing, and a number of other things last year, had really kept flu cases down.”
Plus, although younger New Jerseyans are less likely to be hospitalized or die from Omicron-variant COVID, health officials have observed “significant symptoms” in school-aged children, as well as an increase in both COVID-related hospitalizations and death.
“That is likely just related to the sheer number of people who are now becoming infected with at first Delta, and now the Omicron variant,” Adinaro said. “Cases are not coming down yet.”
Unvaccinated, including young children, at greatest risk
Although some 85 percent of New Jerseyans has received at least one dose of a COVID-19 vaccine, the remaining 15 percent of the population that is unvaccinated accounts for the majority of those people hospitalized with the virus, Adinaro said.
“While it appears that, to an individual, Omicron may cause less serious disease [than Delta], it still has the ability to cause very serious disease,” he said. “Those who are not immunized still remain at significant risk of being hospitalized and potentially dying.”
School-aged children comprise the largest demographic of New Jerseyans who have not yet been vaccinated against COVID-19,” Adinaro said, adding, “It is never too late to start the vaccine.”
Although Omicron seems to be better at evading antibodies than Delta was, Adinaro said that those who recover from an Omicron-variant COVID-19 case “are showing good antibody response and potential immunity to the other types of variants, including Delta.
“What is yet unknown is a) how much that will benefit them if Omicron out-competes Delta, and b) whether people who have been exposed to Omicron would develop “a significant [immune] response” that would make them less likely to be reinfected with Omicron, which makes vaccination and boosters a priority,” he said.
“You may have been infected with COVID in the past, but the importance of getting the vaccine has never been more relevant,” Adinaro said.
“Those who’ve recently received their boosters are showing pretty high levels of protection from symptomatic disease at levels that are comparable to the protection we were seeing against Delta with a primary series,” he said.
And the Omicron-variant wave has yet to top off.
“I think you don’t know if you’re at the peak until you start seeing your numbers go down,” Adinaro said. “COVID is not going away. What it looks like in the future, we don’t know yet, but I think it’s fairly safe to say it’s going to be with us for a long time.”
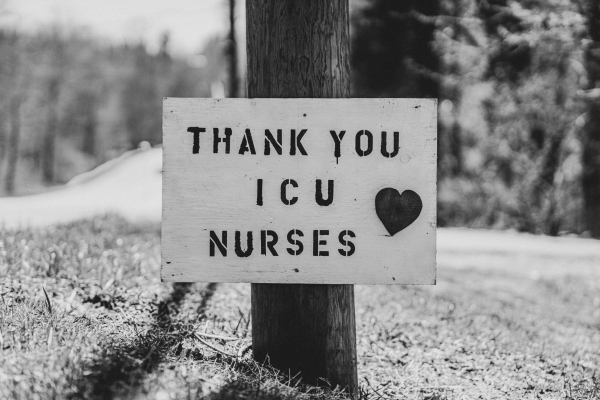
‘Thank you’ sign nailed to a telephone pole, celebrating ICU nurses during the Coronavirus pandemic of 2019/2020.
Photo by Nicholas Bartos on Unsplash
Case overload, staffing shortages threaten ‘a double hit’ for hospitals
The spike in patients threatens New Jersey hospitals with “a double hit” at a time when they have limited resources to pick up the slack.
“Most health care settings were short nurses before the pandemic started [and] they were very short of nurses before this wave started,” Adinaro said.
“We’ve lost nurses and haven’t replaced them… and then if you’re taking a certain percentage of them out of action because they’re sick with Omicron… that is causing a large problem,” he said.
In the spring of 2020, hospitals were able to call upon travel nurses, federal workers, retirees, student nurses, and those from temporarily shuttered surgery centers to make up for a staffing deficit that preceded the pandemic.
“Those pools are not necessarily going to be available this time around,” Adinaro said, “but we do have some resources. The New Jersey National Guard are going to be supporting operations in a number of long-term care (LTC) facilities starting in the next few weeks.”
“If it was just the fact that a large number of healthcare centers… are seeing a significant portion of their staff out sick, or it was that we’re getting a very large influx of patients that are rivaling the numbers we saw last winter… either one of those would be less serious than having both of them at the same time,” Adinaro said.
“Our ICU and ventilator capacity may not be overwhelmed, but the rest of the hospital is likely to be overwhelmed.”
The same staff outages that have hamstrung hospitals during the Omicron-variant surge have also affected other aspects of the pandemic response, from the manufacturers of COVID-19 test kits, to the logistical companies that deliver them, to the laboratories that process the results. Each has been working to overcome workforce depletions owing to the virus; taken together, those shortfalls are delaying several phases of the fight against it.
“Whether it’s schools, the laboratories, or delivery companies, as more workers are sick, their abilities to maintain regular operations are being seriously affected,” Adinaro said.
COVID-19 vaccine bottle mock-up. Photo by Daniel Schludi on Unsplash
Alternative COVID-19 therapies reserved for the immunocompromised
In addition to mitigation strategies like masking and social distancing, Adinaro also advised residents to get vaccinated, particularly because alternative COVID-19 therapeutics are in limited supply.
These pharmaceuticals are being reserved for individuals who are “significantly immunocompromised and may not mount an adequate response to the vaccine,” including people who’ve had solid organ transplants, or who are undergoing cancer treatments.
“We distribute them currently to about 90 different sites every week, and the state does not possess these medications,” Adinaro said. “They’re distributed through a partnership with the federal government, so we’re not stockpiling anything in New Jersey.
Further compounding those stresses: only one of three existing monoclonal antibody therapies has been shown to be effective against Omicron, Adinaro said.
The small allocation of these oral antiviral drugs that New Jersey has received is available at about 24 Walgreens pharmacy locations throughout the state, he said, but it’s to be used exclusively for the early treatment of COVID-positive patients who are at a high risk of hospitalization or death from another health complication.
“We’re really asking the providers that are administering them or prescribing them to really focus on individuals who are at high risk, including those with diabetes, hypertension, and morbid obesity,” Adinaro said.
“They’re not really there for reducing significant symptomatic disease.”
Does Omicron signal the transition from pandemic to endemic COVID?
One of the few opportunities for optimism in the surging wave of Omicron-variant COVID-19 has been the hope that it may foretell the pandemic winding down into weaker-strength iterations of the virus that are more survivable.
Although Adinaro said Omicron may be the endemic variant of choice over Delta, there still are no guarantees that COVID-19 won’t continue to evolve into something worse.
“When Delta became dominant, if you had told us that there would be another variant that would become dominant in a few weeks, rather than a few months, [after] coming into a country, I don’t think we would have expected that,” Adinaro said.
“Since Omicron, there are several other variants that have been identified that haven’t made it to the level of being a variant of concern, but I think it’s always possible,” he said. “It would be impressive to find another variant that would be more infectious than Omicron.”
Whether a less-severe version of COVID-19 could foretell the end of the pandemic, general fatigue at the prospect of a third year of widespread infections has left many people either hypervigilant against any COVID-related risks, or abandoning reasonable precautions out of a sense of hopelessness. Adinaro said that’s to be expected when it’s unknown if the end is in sight.
“I think people are great at gearing up for things when they know that there’s an endpoint, and I can understand people’s fatigue in not fully understanding what’s the destination, or when we get to that endemic point, where we figure out how to live with that,” he said.
“How do we get people to continue to do things once they’re tired?”